Mandibular Growth after Orthognathic Surgery: A Case Report and Clinical Implications
- Dr. Park

- Nov 1, 2024
- 4 min read
During consultations, many patients still express concerns about the side effects of orthognathic surgery. While even double eyelid surgery carries the risk of serious complications like blindness, most patients perceive orthognathic surgery as a riskier procedure. Considering factors such as operation time and blood loss, this perception is not entirely inaccurate.
Patients are often most concerned about common side effects like postoperative sensory disturbances and relapse.
In cases of mandibular prognathism, surgical relapse or recurrence can result in the mandible not settling in the planned position, potentially affecting the final occlusion after orthodontic treatment.
This refers to the biological process where bone remodels and adapts in response to altered mechanical loading or environmental changes. In the context of orthognathic surgery, changes in jaw position and muscle function could induce adaptive growth in the mandible.
However, it is questionable whether this phenomenon should be considered a side effect if it is caused by physiological mandibular growth.
This raises the question:
Can bone growth occur after orthognathic surgery?
It's true that if the mandible continues to grow physiologically after surgery, leading to a less than ideal final outcome, it might be inaccurate to label it as a "complication" or "side effect." This is because the growth may be a natural process, not directly caused by the surgery itself.
Perhaps, in these cases, it might be more appropriate to consider this phenomenon as a "growth-related change" than "post-surgical adaptation."
Today, I'd like to share my clinical experience regarding this topic.
Case Presentation
This case involves a male patient in his early 20s who underwent surgery-first orthognathic surgery, followed by orthodontic treatment. Postoperative orthodontics was completed 1 year and 6 months after surgery.
Preoperatively, an anterior open bite is observed.
The mandibular prognathism was corrected surgically.


Preoperative and Postoperative Occlusion

What is Relapse or Recurrence after Orthognathic Surgery?
Relapse or recurrence typically refers to a return towards the original condition. In prognathic cases, this means the mandible protrudes again, and in retrognathic cases, the mandible retrudes.
Some hypotheses attribute this to soft tissue adaptation to rapid skeletal changes or the tendency of muscles to return to their original positions.
My clinical experience suggests that in prognathic cases, the temporalis and masseter muscles, when lengthened, tend to return to their original length. Therefore, surgical planning should aim to minimize stretching of these muscles.
Another hypothesis is the potential for residual growth in patients undergoing orthognathic surgery for mandibular prognathism, even after the age of 20.
It remains unclear whether this residual growth is triggered by the surgery itself or if it's a natural physiological phenomenon that has become more apparent with the widespread use of precise measurement tools like CT scans.
To my knowledge, there are no published studies that have used CT scans to measure facial skeletal changes in individuals over 20 years old.
To assess changes in skeletal dimensions over time, we compared cephalometric measurements at 5 weeks postoperatively (when condylar sagging had mostly resolved) and at 1 year and 6 months postoperatively.
Comparison of 5 Weeks Postoperative and 1 Year 6 Months Postoperative
The pogonion has moved 2.04 mm anteriorly compared to its position at 5 weeks postoperatively. This phenomenon can be attributed to autorotation of the mandible due to occlusal seating. However, as shown, the vertical position of the pogonion has actually moved slightly downward. If the rotation had occurred around the condyle, the vertical position of the pogonion should have moved upward.

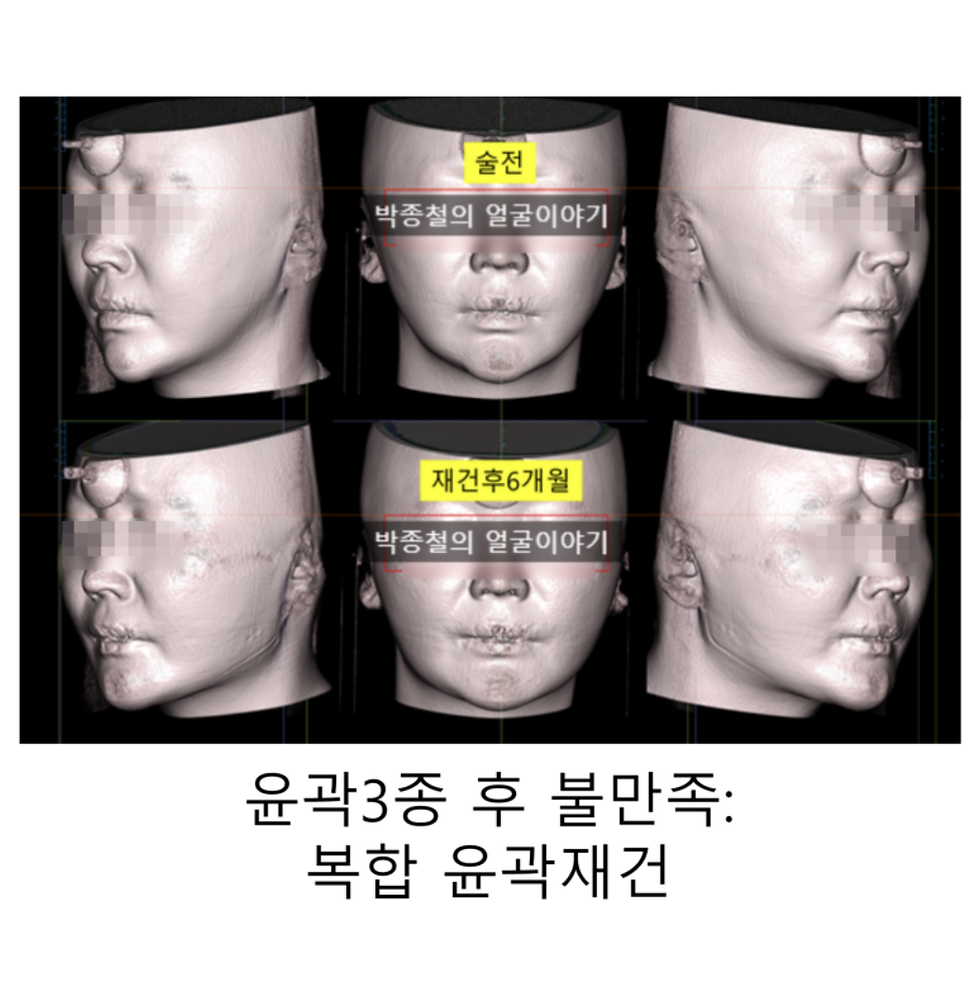
Superimposition of 5 Weeks Postoperative and 1 Year 6 Months Postoperative Skeletal Structures The mandible appears to be positioned more anteriorly overall at 1 year and 6 months postoperatively. However, this could also be due to the posteriorly positioned condyle returning to its original location. Therefore, we examined the position of the condyle in the temporomandibular joint.

No significant difference is observed.
Next, we measured the actual distance from the condyle to the pogonion.The distance from the condyle to the pogonion was 122.89 mm at 5 weeks postoperatively and increased to 124.28 mm at 1 year and 6 months postoperatively, indicating an approximate increase of 1.39 mm. The lateral superimposition image also shows that the mandible is more anterior at 1 year and 6 months postoperatively.
Given the increased length, it is more accurate to describe this as anterior mandibular growth rather than just anterior movement.

Mandibular Growth after Orthognathic Surgery: A Case Report and Clinical Implications
Therefore, when planning surgical occlusion for patients in their early 20s undergoing orthognathic surgery, I take this potential for growth into account.

Key Points:
postoperative mandibular growth can occur in patients in their early 20s, potentially affecting treatment outcomes.
This growth may be due to residual growth potential or other factors.
If this postoperative mandibular growth is observed in individuals over 20 years of age, it could be generally categorized as adaptive growth or compensatory growth commonly seen after orthognathic surgery.
However, if this phenomenon is predominantly observed in patients in their early 20s, it might be more accurately described as residual growth or late mandibular growth.
Careful planning and consideration of this potential growth are essential for successful orthognathic surgery in this age group.
for more information:
Here's a more detailed explanation of these terms :
Adaptive Growth: This refers to the biological process where bone remodels and adapts in response to altered mechanical loading or environmental changes. In the context of orthognathic surgery, changes in jaw position and muscle function could induce adaptive growth in the mandible. This type of growth can occur at any age, although it might be more pronounced in younger individuals with greater growth potential.
Compensatory Growth: This describes growth that occurs to compensate for a deficiency or loss of bone tissue. While less common in routine orthognathic procedures, compensatory growth might be observed if there is any bone removal or alteration in the temporomandibular joint during surgery. Similar to adaptive growth, compensatory growth can also occur throughout life.
Residual Growth: This term specifically refers to the continuation of growth after the main growth spurt has subsided. While skeletal maturity is typically reached in late adolescence, some individuals may exhibit residual growth in their early 20s. This could explain why postoperative mandibular growth might be more prevalent in this age group.
Late Mandibular Growth: This emphasizes the occurrence of mandibular growth beyond the expected timeframe of adolescence. It acknowledges that mandibular growth can extend into the early 20s and potentially even later, although the extent and clinical significance of this late growth require further investigation.


Comments